You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
The shadow
The shadow knows!
Republican state lawmakers vote to overturn statewide mask mandate
Covid likes this.
Covid likes this.
The shadow
The shadow knows!
nivek
As Above So Below
Pandemic allows drug-resistant bacteria to take hold
As COVID-19 took hold over the past year, hospitals and nursing homes used and reused scarce protective equipment — masks, gloves, gowns. This desperate frugality helped prevent the airborne transfer of the virus. But it also appears to have helped spread a different set of germs — drug-resistant bacteria and fungi — that have used the chaos of the pandemic to grow opportunistically in health care settings around the globe.
These bacteria and fungi, like COVID-19, prey on older people, the infirm and those with compromised immune systems. They can cling tenaciously to clothing and medical equipment, which is why nursing homes and hospitals before the pandemic were increasingly focused on cleaning rooms and changing gowns to prevent their spread.
That emphasis all but slipped away amid an all-consuming focus on the coronavirus. In fact, experts warn, the changes in hygiene and other practices caused by the COVID-19 fight are likely to have contributed to the spread of these drug-resistant germs.
“Seeing the world as a one-pathogen world is really problematic,” said Dr. Susan S. Huang, an infectious disease specialist at the University of California at Irvine Medical School, noting that the nearly singular focus on the pandemic appears to have led to more spread of drug-resistant infection. “We have every reason to believe the problem has gotten worse.”
A few data points reinforce her fears, including isolated outbreaks of various drug-resistant infections in Florida, New Jersey and California, as well as in India, Italy, Peru and France. Overall figures have been hard to track because many nursing homes and hospitals simply stopped screening for the germs as resources were diverted to COVID-19.
When even modest screening picked up again early in the summer, the results suggested that certain drug-resistant organisms had taken root and spread. Particularly troublesome have been growing case counts of a fungus called Candida auris, which authorities had tried to fight before the pandemic with increased screening, isolation of infected patients and better hygiene.
These intensive efforts had limited the spread of C. auris to a handful of cases in Los Angeles County. Now there are around 250, said Dr. Zachary Rubin, who leads the county’s infection control efforts at health care facilities. “We saw a blooming in Candida auris,” said Rubin, who attributed the change to a handful of factors, notably the challenges in testing for the germ when so many testing resources went toward COVID-19.
Noxious drug-resistant bacteria are surfacing too, including Carbapenem-resistant Acinetobacter baumannii, which is considered an “urgent health threat” by the Centers for Disease Control and Prevention. In December, the CDC reported a cluster of Acinetobacter baumannii during a surge of COVID-19 patients in an urban New Jersey hospital with about 500 beds. The hospital was not identified. And hospitals in Italy and Peru saw the spread of the bacteria Klebsiella pneumoniae.
In an acknowledgment of the issue, three major medical societies sent a letter Dec. 28 to the Centers for Medicare and Medicaid Services asking for a temporary suspension of rules that tie reimbursement rates to hospital-acquired infections. The three groups — the Society of Healthcare Epidemiology of America, the Society of Infectious Diseases Pharmacists and the Association for Infection Control and Epidemiology — feared that the infection rates may have risen because of COVID-19.
“Patient care staffing, supplies, care sites and standard practices have all changed during this extraordinary time,” the letter stated.
Not all types of drug-resistant infections have risen. For instance, some research shows no particular change during the pandemic in the rate of hospital patients acquiring the bacterium Clostridioides difficile — a finding that suggests the overall long-term effect of the pandemic on these infections is not yet clear.
Huang and other experts said they are not suggesting that the priority on fighting COVID-19 was misplaced. Rather, they say that renewed attention must be paid to drug-resistant germs. Earlier research has shown that as many as 65% of residents of nursing homes carry some form of drug-resistant infection.
Over the years, critics have charged that hospitals and, in particular, nursing homes, have been lax in their efforts to confront these infections because it is expensive to disinfect equipment, train staff, isolate infected patients and screen for the germs.
In response to these and other concerns, a greater effort was beginning to be made before the pandemic to monitor patients for these infections, particularly as they cycled in and out of nursing homes and intensive care units. This revolving door is known to spread germs that are carried by infected patients.
But after the pandemic began, there was much less monitoring and even, at times, a wholesale breakdown of communications about the transfer of such patients, experts said. Plus, the sickest COVID-19 patients were put on ventilators, where drug-resistant infections can cling and then spread.
Another possible contributor has been the heavy and regular use of steroids to treat COVID-19. These drugs help alleviate the virus’s most dangerous symptoms but can leave the immune system compromised in a way that allows other germs to more easily infiltrate the body.
The combination of these factors “is perfect” for the fungus to “take hold,” said Dr. Tom Chiller, the head of the fungal division of the CDC.
Earlier this month, the Florida Department of Health published a case report of four Candida auris cases at a hospital in Florida. (The hospital’s identity is masked by the CDC and the state). In an effort to understand the spread, the Florida department of health visited the COVID unit there in August. Their inquiry found that 35 of 67 patients admitted to the unit from Aug. 4 to 18 were colonized with C. auris, meaning that the fungus was on their skin but they were not yet infected. Subsequently, six of the patients became infected.
Crucially, the study found that the spread of the fungus from one patient to the next may well have come from health care providers carrying the germ on protective gowns or gloves, as well as on mobile computers and other equipment that had been insufficiently cleaned. This was, the CDC and other experts said, a breakdown in infection control, a practice that had come under intense scrutiny in 2019 after C. auris took root in the East Coast and began to spread.
Nationally, the number of infections had increased to around 1,625 by November 2020, from 952 since the end of October 2019. The current number is likely far higher, Chiller said, because screening for the germ was largely halted early in the pandemic. When it picked up again, the numbers rose to 83 infections in August and 195 patients colonized — and, even then, testing was not as widespread as pre-pandemic.
The upshot is that the confirmed cases are “likely the tip of the iceberg,” Chiller said.
.
As COVID-19 took hold over the past year, hospitals and nursing homes used and reused scarce protective equipment — masks, gloves, gowns. This desperate frugality helped prevent the airborne transfer of the virus. But it also appears to have helped spread a different set of germs — drug-resistant bacteria and fungi — that have used the chaos of the pandemic to grow opportunistically in health care settings around the globe.
These bacteria and fungi, like COVID-19, prey on older people, the infirm and those with compromised immune systems. They can cling tenaciously to clothing and medical equipment, which is why nursing homes and hospitals before the pandemic were increasingly focused on cleaning rooms and changing gowns to prevent their spread.
That emphasis all but slipped away amid an all-consuming focus on the coronavirus. In fact, experts warn, the changes in hygiene and other practices caused by the COVID-19 fight are likely to have contributed to the spread of these drug-resistant germs.
“Seeing the world as a one-pathogen world is really problematic,” said Dr. Susan S. Huang, an infectious disease specialist at the University of California at Irvine Medical School, noting that the nearly singular focus on the pandemic appears to have led to more spread of drug-resistant infection. “We have every reason to believe the problem has gotten worse.”
A few data points reinforce her fears, including isolated outbreaks of various drug-resistant infections in Florida, New Jersey and California, as well as in India, Italy, Peru and France. Overall figures have been hard to track because many nursing homes and hospitals simply stopped screening for the germs as resources were diverted to COVID-19.
When even modest screening picked up again early in the summer, the results suggested that certain drug-resistant organisms had taken root and spread. Particularly troublesome have been growing case counts of a fungus called Candida auris, which authorities had tried to fight before the pandemic with increased screening, isolation of infected patients and better hygiene.
These intensive efforts had limited the spread of C. auris to a handful of cases in Los Angeles County. Now there are around 250, said Dr. Zachary Rubin, who leads the county’s infection control efforts at health care facilities. “We saw a blooming in Candida auris,” said Rubin, who attributed the change to a handful of factors, notably the challenges in testing for the germ when so many testing resources went toward COVID-19.
Noxious drug-resistant bacteria are surfacing too, including Carbapenem-resistant Acinetobacter baumannii, which is considered an “urgent health threat” by the Centers for Disease Control and Prevention. In December, the CDC reported a cluster of Acinetobacter baumannii during a surge of COVID-19 patients in an urban New Jersey hospital with about 500 beds. The hospital was not identified. And hospitals in Italy and Peru saw the spread of the bacteria Klebsiella pneumoniae.
In an acknowledgment of the issue, three major medical societies sent a letter Dec. 28 to the Centers for Medicare and Medicaid Services asking for a temporary suspension of rules that tie reimbursement rates to hospital-acquired infections. The three groups — the Society of Healthcare Epidemiology of America, the Society of Infectious Diseases Pharmacists and the Association for Infection Control and Epidemiology — feared that the infection rates may have risen because of COVID-19.
“Patient care staffing, supplies, care sites and standard practices have all changed during this extraordinary time,” the letter stated.
Not all types of drug-resistant infections have risen. For instance, some research shows no particular change during the pandemic in the rate of hospital patients acquiring the bacterium Clostridioides difficile — a finding that suggests the overall long-term effect of the pandemic on these infections is not yet clear.
Huang and other experts said they are not suggesting that the priority on fighting COVID-19 was misplaced. Rather, they say that renewed attention must be paid to drug-resistant germs. Earlier research has shown that as many as 65% of residents of nursing homes carry some form of drug-resistant infection.
Over the years, critics have charged that hospitals and, in particular, nursing homes, have been lax in their efforts to confront these infections because it is expensive to disinfect equipment, train staff, isolate infected patients and screen for the germs.
In response to these and other concerns, a greater effort was beginning to be made before the pandemic to monitor patients for these infections, particularly as they cycled in and out of nursing homes and intensive care units. This revolving door is known to spread germs that are carried by infected patients.
But after the pandemic began, there was much less monitoring and even, at times, a wholesale breakdown of communications about the transfer of such patients, experts said. Plus, the sickest COVID-19 patients were put on ventilators, where drug-resistant infections can cling and then spread.
Another possible contributor has been the heavy and regular use of steroids to treat COVID-19. These drugs help alleviate the virus’s most dangerous symptoms but can leave the immune system compromised in a way that allows other germs to more easily infiltrate the body.
The combination of these factors “is perfect” for the fungus to “take hold,” said Dr. Tom Chiller, the head of the fungal division of the CDC.
Earlier this month, the Florida Department of Health published a case report of four Candida auris cases at a hospital in Florida. (The hospital’s identity is masked by the CDC and the state). In an effort to understand the spread, the Florida department of health visited the COVID unit there in August. Their inquiry found that 35 of 67 patients admitted to the unit from Aug. 4 to 18 were colonized with C. auris, meaning that the fungus was on their skin but they were not yet infected. Subsequently, six of the patients became infected.
Crucially, the study found that the spread of the fungus from one patient to the next may well have come from health care providers carrying the germ on protective gowns or gloves, as well as on mobile computers and other equipment that had been insufficiently cleaned. This was, the CDC and other experts said, a breakdown in infection control, a practice that had come under intense scrutiny in 2019 after C. auris took root in the East Coast and began to spread.
Nationally, the number of infections had increased to around 1,625 by November 2020, from 952 since the end of October 2019. The current number is likely far higher, Chiller said, because screening for the germ was largely halted early in the pandemic. When it picked up again, the numbers rose to 83 infections in August and 195 patients colonized — and, even then, testing was not as widespread as pre-pandemic.
The upshot is that the confirmed cases are “likely the tip of the iceberg,” Chiller said.
.
nivek
As Above So Below
Johnson & Johnson COVID-19 vaccine 66% effective in global trial, company says
Johnson & Johnson on Friday said its single-shot coronavirus vaccine was 72% effective in preventing moderate-to-severe COVID-19 in the U.S, but fell to 66% in a larger trial conducted worldwide. The results stem from a Phase 3 ENSEMBLE clinical trial, which involved 43,783 participants.
The shot was found to be 66% effective in preventing moderate-to-severe illness in Latin America, and 57% effective in South Africa at 28 days post-vaccination. When the company only looked at severe cases, protection rose to 85%.
J&J’s vaccine differs from currently approved jabs in the U.S. in that it requires a single shot as opposed to two doses, and was created using an adenovirus rather than mRNA technology.
"Johnson & Johnson embarked on the global effort to combat the COVID-19 pandemic a year ago, and has brought the full force of our capabilities, as well as tremendous public-private partnerships, to enable the development of a single-shot vaccine. Our goal all along has been to create a simple, effective solution for the largest number of people possible, and to have maximum impact to help end the pandemic," Alex Gorsky, Chairman, Board of Directors and Chief Executive Officer, Johnson & Johnson said in a press release Friday. "We’re proud to have reached this critical milestone and our commitment to address this global health crisis continues with urgency for everyone, everywhere."
The company suggested the shot was safe and well-tolerated; 9% of trial participants developed a fever and there were no serious allergic reactions.
J&J also boosted hopes its vaccine candidate will be effective against variant strains.
"Protection was generally consistent across race, age groups, including adults over 60 years of age (N= 13,610), and across all variants and regions studied, including South Africa where nearly all cases of COVID-19 (95%) were due to infection with a SARS-CoV-2 variant from the B.1.351 lineage," reads the release.
The company said it plans to file for an emergency use authorization (EUA) in the U.S. in early February, with product ready to ship immediately after authorization. The company expects the vaccine to remain stable for two years at minus 20 degrees Celsius, and at least three months at 2 degrees Celsius to 8 degrees Celsius.
(More on the link)
.
Johnson & Johnson on Friday said its single-shot coronavirus vaccine was 72% effective in preventing moderate-to-severe COVID-19 in the U.S, but fell to 66% in a larger trial conducted worldwide. The results stem from a Phase 3 ENSEMBLE clinical trial, which involved 43,783 participants.
The shot was found to be 66% effective in preventing moderate-to-severe illness in Latin America, and 57% effective in South Africa at 28 days post-vaccination. When the company only looked at severe cases, protection rose to 85%.
J&J’s vaccine differs from currently approved jabs in the U.S. in that it requires a single shot as opposed to two doses, and was created using an adenovirus rather than mRNA technology.
"Johnson & Johnson embarked on the global effort to combat the COVID-19 pandemic a year ago, and has brought the full force of our capabilities, as well as tremendous public-private partnerships, to enable the development of a single-shot vaccine. Our goal all along has been to create a simple, effective solution for the largest number of people possible, and to have maximum impact to help end the pandemic," Alex Gorsky, Chairman, Board of Directors and Chief Executive Officer, Johnson & Johnson said in a press release Friday. "We’re proud to have reached this critical milestone and our commitment to address this global health crisis continues with urgency for everyone, everywhere."
The company suggested the shot was safe and well-tolerated; 9% of trial participants developed a fever and there were no serious allergic reactions.
J&J also boosted hopes its vaccine candidate will be effective against variant strains.
"Protection was generally consistent across race, age groups, including adults over 60 years of age (N= 13,610), and across all variants and regions studied, including South Africa where nearly all cases of COVID-19 (95%) were due to infection with a SARS-CoV-2 variant from the B.1.351 lineage," reads the release.
The company said it plans to file for an emergency use authorization (EUA) in the U.S. in early February, with product ready to ship immediately after authorization. The company expects the vaccine to remain stable for two years at minus 20 degrees Celsius, and at least three months at 2 degrees Celsius to 8 degrees Celsius.
(More on the link)
.
nivek
As Above So Below
First known U.S. cases of potent South African COVID-19 variant found in South Carolina
A potent coronavirus variant originating in South Africa and found to be partly resistant to current vaccines and antibody treatments has been detected for the first time in the United States in two South Carolina patients, health officials said on Thursday.
Medical experts said arrival of the so-called South African variant presented an alarming new challenge in efforts to contain a raging pandemic that has claimed at least 430,000 American lives in 11 months, as authorities struggle to launch the largest mass-vaccination campaign in U.S. history.
All viruses mutate frequently, and scientists have identified several variants of the novel coronavirus found to be more transmissible than the original strain.
But the presence of the South African variant, which has shown no evidence of causing more severe disease, is nonetheless especially concerning because several laboratory studies have found that it reduces vaccine and antibody therapy efficacy.
Confirmation of two patients with that variant in South Carolina came days after the Minnesota Department of Health identified the first known U.S. case of another highly contagious strain that originated in Brazil.
Yet a third form of the virus from the UK that is more infectious, and associated with higher mortality, made its first U.S. appearance last month in Colorado and has since been detected in at least 28 states.
The flurry of variants taken together "have really changed the entire picture of the COVID-19 pandemic," Dr. Michael Osterholm, director of the University of Minnesota's Center for Infectious Disease Research and Policy, said in an MSNBC interview. "We're now in by far the most dangerous period of the pandemic."
The U.S. Centers for Disease Control and Prevention (CDC) has predicted the UK variant could become the dominant strain in the United States by March.
(More on the link)
.
A potent coronavirus variant originating in South Africa and found to be partly resistant to current vaccines and antibody treatments has been detected for the first time in the United States in two South Carolina patients, health officials said on Thursday.
Medical experts said arrival of the so-called South African variant presented an alarming new challenge in efforts to contain a raging pandemic that has claimed at least 430,000 American lives in 11 months, as authorities struggle to launch the largest mass-vaccination campaign in U.S. history.
All viruses mutate frequently, and scientists have identified several variants of the novel coronavirus found to be more transmissible than the original strain.
But the presence of the South African variant, which has shown no evidence of causing more severe disease, is nonetheless especially concerning because several laboratory studies have found that it reduces vaccine and antibody therapy efficacy.
Confirmation of two patients with that variant in South Carolina came days after the Minnesota Department of Health identified the first known U.S. case of another highly contagious strain that originated in Brazil.
Yet a third form of the virus from the UK that is more infectious, and associated with higher mortality, made its first U.S. appearance last month in Colorado and has since been detected in at least 28 states.
The flurry of variants taken together "have really changed the entire picture of the COVID-19 pandemic," Dr. Michael Osterholm, director of the University of Minnesota's Center for Infectious Disease Research and Policy, said in an MSNBC interview. "We're now in by far the most dangerous period of the pandemic."
The U.S. Centers for Disease Control and Prevention (CDC) has predicted the UK variant could become the dominant strain in the United States by March.
(More on the link)
.
nivek
As Above So Below
Johnson & Johnson's COVID-19 Vaccine Results Are Better Than They May Sound
Johnson & Johnson’s Janssen Pharmaceutical Companies announced on Jan. 29 that its one-shot COVID-19 vaccine is 66% effective in protecting against disease, but 85% effective against preventing severe disease—results that could make it especially valuable in the effort to vaccinate parts of the world with weak health care systems.
By comparison, the vaccines already authorized in the U.S.—one from Moderna and one from Pfizer-BioNTech—each require two doses, spaced three to four weeks apart. Janssen’s vaccine can also be stored in normal refrigerators, unlike Moderna’s and Pfizer-BioNTech’s, both of which need to be frozen. While the vaccines from Moderna and Pfizer-BioNTech are around 94%-95% effective in protecting against COVID-19, that’s after two doses of those shots, which are based on mRNA, a relatively new vaccine platform. Janssen’s vaccine relies on a more traditional approach: it uses a harmless human cold virus to deliver a SARS-CoV-2 gene to the human immune system, which then learns to protect the body against COVID-19. (SARS-CoV-2 is the virus that causes COVID-19.)
“A one-shot vaccine is considered by the World Health Organization to be the best option in pandemic settings, enhancing access, distribution and compliance,” said J&J Chief Science Officer Dr. Paul Stoffels in a statement. “85% efficacy in preventing severe COVID-19 disease and prevention of COVID-19-related medical interventions will potentially protect hundreds of millions of people from serious and fatal outcomes of COVID-19.”
The J&J results came a few days after Maryland-based Novavax reported that, in a Phase 3 trial, its vaccine was nearly 90% effective in protecting against COVID-19 disease. Those results are especially reassuring since that study was conducted among 15,000 people in the U.K., where a new mutant variant of SARS-CoV-2 is quickly gaining hold. The high efficacy suggests that people vaccinated with the Novavax shot, which is based on another proven technology of injecting proteins made by SARS-CoV-2 to stimulate an immune response, can expect good protection against that new variant.
(More on the link)
.
Johnson & Johnson’s Janssen Pharmaceutical Companies announced on Jan. 29 that its one-shot COVID-19 vaccine is 66% effective in protecting against disease, but 85% effective against preventing severe disease—results that could make it especially valuable in the effort to vaccinate parts of the world with weak health care systems.
By comparison, the vaccines already authorized in the U.S.—one from Moderna and one from Pfizer-BioNTech—each require two doses, spaced three to four weeks apart. Janssen’s vaccine can also be stored in normal refrigerators, unlike Moderna’s and Pfizer-BioNTech’s, both of which need to be frozen. While the vaccines from Moderna and Pfizer-BioNTech are around 94%-95% effective in protecting against COVID-19, that’s after two doses of those shots, which are based on mRNA, a relatively new vaccine platform. Janssen’s vaccine relies on a more traditional approach: it uses a harmless human cold virus to deliver a SARS-CoV-2 gene to the human immune system, which then learns to protect the body against COVID-19. (SARS-CoV-2 is the virus that causes COVID-19.)
“A one-shot vaccine is considered by the World Health Organization to be the best option in pandemic settings, enhancing access, distribution and compliance,” said J&J Chief Science Officer Dr. Paul Stoffels in a statement. “85% efficacy in preventing severe COVID-19 disease and prevention of COVID-19-related medical interventions will potentially protect hundreds of millions of people from serious and fatal outcomes of COVID-19.”
The J&J results came a few days after Maryland-based Novavax reported that, in a Phase 3 trial, its vaccine was nearly 90% effective in protecting against COVID-19 disease. Those results are especially reassuring since that study was conducted among 15,000 people in the U.K., where a new mutant variant of SARS-CoV-2 is quickly gaining hold. The high efficacy suggests that people vaccinated with the Novavax shot, which is based on another proven technology of injecting proteins made by SARS-CoV-2 to stimulate an immune response, can expect good protection against that new variant.
(More on the link)
.
nivek
As Above So Below
These vaccination efforts may be futile, this infection reported below could be one of the new variants that are more resistant to our vaccines and could be only the beginning of more similar cases arising...
...
Congressman who had second COVID-19 vaccine dose tests positive for virus
A Massachusetts congressman tested positive coronavirus just a few weeks after receiving the second of two doses of the Pfizer vaccine.
Molly Rose Tarpey, the communications director for Rep. Stephen Lynch, told Fox News on Saturday that the lawmaker received the second jab and tested negative for COVID-19 before attending President Biden's inauguration in Washington, D.C., on Jan. 20.
On Friday, Lynch, D-Mass., received a positive test result for coronavirus after a staff member in his Boston office also contracted the virus.
(More on the link)
.
...
Congressman who had second COVID-19 vaccine dose tests positive for virus
A Massachusetts congressman tested positive coronavirus just a few weeks after receiving the second of two doses of the Pfizer vaccine.
Molly Rose Tarpey, the communications director for Rep. Stephen Lynch, told Fox News on Saturday that the lawmaker received the second jab and tested negative for COVID-19 before attending President Biden's inauguration in Washington, D.C., on Jan. 20.
On Friday, Lynch, D-Mass., received a positive test result for coronavirus after a staff member in his Boston office also contracted the virus.
(More on the link)
.
nivek
As Above So Below
Dangerous new coronavirus strains may incubate in COVID-19's sickest
(Excerpts)
In the U.K. strain, the genetic change known as N501Y is thought to help enhance the virus’ transmissibility by about 50%. In the South Africa strain, it may reduce the effectiveness of COVID-19 vaccines and treatments. Tests of its effect on the Brazil variant are still in progress.
Among the sickest of COVID-19 patients, this population of "long haulers" appears to play a key role in incubating new variants of the coronavirus, some of which could change the trajectory of the pandemic.
The mutations that arose from this single patient are “a microcosm of the viral evolution we’re seeing globally,” said Dr. Jonathan Z. Li, an infectious-disease specialist at Brigham and Women’s Hospital in Boston who treated him. “He showed us what could happen” when a germ with a knack for genetic shape-shifting stumbles upon conditions that reward it for doing so.
Indeed, situations in which patients can’t clear a viral infection are “the worst possible scenario for developing mutations,” said Dr. Bruce Walker, an immunologist and founding director of the Ragon Institute in Boston.
As weeks of illness turn into months, a virus copies itself millions of times. Each copy is an opportunity to make random mistakes. As it spins off new mutations, the virus may happen upon ones that help it resist medications, evade the immune system and come back stronger.
SARS-CoV-2, the coronavirus that causes COVID-19, has been an unpredictable adversary. The chance to witness its transformation in near-real time, and see where and how it mutates in a single host, can guide the design of vaccines and medications that don't lose their effectiveness over time, Walker said.
(More on the link)
.
(Excerpts)
In the U.K. strain, the genetic change known as N501Y is thought to help enhance the virus’ transmissibility by about 50%. In the South Africa strain, it may reduce the effectiveness of COVID-19 vaccines and treatments. Tests of its effect on the Brazil variant are still in progress.
Among the sickest of COVID-19 patients, this population of "long haulers" appears to play a key role in incubating new variants of the coronavirus, some of which could change the trajectory of the pandemic.
The mutations that arose from this single patient are “a microcosm of the viral evolution we’re seeing globally,” said Dr. Jonathan Z. Li, an infectious-disease specialist at Brigham and Women’s Hospital in Boston who treated him. “He showed us what could happen” when a germ with a knack for genetic shape-shifting stumbles upon conditions that reward it for doing so.
Indeed, situations in which patients can’t clear a viral infection are “the worst possible scenario for developing mutations,” said Dr. Bruce Walker, an immunologist and founding director of the Ragon Institute in Boston.
As weeks of illness turn into months, a virus copies itself millions of times. Each copy is an opportunity to make random mistakes. As it spins off new mutations, the virus may happen upon ones that help it resist medications, evade the immune system and come back stronger.
SARS-CoV-2, the coronavirus that causes COVID-19, has been an unpredictable adversary. The chance to witness its transformation in near-real time, and see where and how it mutates in a single host, can guide the design of vaccines and medications that don't lose their effectiveness over time, Walker said.
(More on the link)
.
nivek
As Above So Below
What to know about 4 worrisome coronavirus variants, including one that can partially evade vaccines
While mutations are normal and most don't change a virus's behavior, sometimes these genetic errors give the virus an evolutionary leg-up against its hosts - mutations that make it more infectious, deadlier, or perhaps able to evade the protective immunity we accrue from vaccines or prior infections.
Since the fall, researchers have identified worrisome mutated strains spreading worldwide, many of which are nicknamed after where they were first detected. Many of these variants - including those from the UK, South Africa, and Brazil - share similar mutations in their spike proteins, which is what the virus uses to invade human cells. Research suggests those genetic tweaks may make it easier for the strains to infect people; some may decrease the efficacy of vaccines.
"We can see that we are going to be challenged" by the variant from South Africa, the US's leading infectious disease expert Dr. Anthony Fauci said in a press call on Friday.
Here's what to know about four coronavirus variants, where they've been spotted, and what they mean for global vaccination efforts.
B.1.1.7, the variant first spotted in the UK
Researchers spotted the first variant of concern, named B.1.1.7, in the southeastern part of the UK on September 20. By mid-December, it had overtaken all other versions of the virus in the country. B.1.1.7 is now present in 70 countries; US officials have spotted 315 cases in 28 states.
Studies have shown B.1.1.7 is between 56% and 70% more contagious than its viral predecessors. While initial evidence suggested the strain wasn't deadlier, UK officials said last week people infected with B.1.1.7 may face a higher risk of death than those who get other strains. The World Health Organization and other experts, however, cautioned more data was needed to confirm whether the variant was associated with higher mortality.
What makes B.1.1.7 so pernicious is that people infected with B.1.1.7 have higher viral loads, meaning they produce more viral particles when they're infected. Higher viral loads, multiple studies show, are associated with a higher risk of death and more severe disease.
The variant has at least 17 mutations. But two are among the most concerning because they affect its spike protein shape and may increase transmissibility: the swapping of two amino acids in the 501st position of its genome, or N501Y, and a deletion of amino acids in its 69th and 70th positions, known as the 69/70 deletion.
Virologists think vaccines will still be effective against B.1.1.7, and recent research from Pfizer-BioNTech and Moderna found that the companies' shots held up well against that variant.
Novavax, too, said Thursday its vaccine was 89% effective at preventing cases of COVID-19 based on results from a UK trial, which suggests it works against B.1.1.7.
B.1.351, the variant first found in South Africa
Experts agree the variant first detected in South Africa in October, known as B.1.351 (or 501.Y.V2), is more worrisome than the variant first found in the UK.
This variant also has the N501Y mutation, though it lacks the worrisome 69/70 deletion. But what makes this strain troublesome is two spike mutations - K417T and E484K - that are missing in B.1.1.7. E484K, in particular, has been shown to reduce how well antibodies - proteins that identify and help destroy pathogens - can recognize the coronavirus.
B.1.351 has spread to 31 countries. The US reported its first two cases of the variant, which is 50% more transmissible, Thursday.
While there's no evidence it is deadlier or causes more severe COVID-19, preliminary research published last week suggested the variant can partially evade the defenses existing vaccines build in our bodies' immune systems.
Vaccine developers Novavax and Johnson & Johnson announced Friday that their shots didn't work as well against B.1.351 than other strains. Novavax's vaccine was 89% effective at preventing COVID-19 cases in the UK, but only 49% effective in South Africa, where B.1351 is the dominant version of the virus. J&J found its shot was, on average, 66% effective; that efficacy dropped to 57% in South Africa.
Though even with the variant concerns, J&J said its vaccine was 85% effective at preventing severe COVID-19 across all geographic regions - the UK, US, Latin America, and South Africa - in which it conducted clinical trials.
Following lab research, Pfizer and Moderna, both say their vaccines will work again B.1.351. Yet recent preliminary data from Moderna showed blood samples taken from vaccinated people that were infected with B.1.351 developed six times fewer virus-neutralizing antibodies than samples exposed to other variants.
This suggests vaccines won't provide as much protection against B.1.351, and people who have already been infected with a different version of the virus could get reinfected with the new strain. (However, this lab testing doesn't take into account other elements of immunity beyond antibodies, like virus-destroying T cells.)
P.1, the variant from Brazil
A variant named P.1, with a similar genetic profile to B.1.351, is surging in Brazil. In mid-December, 42% of coronavirus cases in the Amazon region involved P.1.
Researchers first detected this strain in four travelers from Brazil who had traveled to Japan's Haneda airport outside Tokyo. Data show it's 50% more transmissible that the original version of the virus, and has the same trio of concerning spike mutations as B.1.351: N501Y, K417T, and E484K, so may also be able to evade antibodies generated from previous infections or a vaccine.
A study from earlier in January pinpointed P.1 as a variant of concerning after finding that cases had started spiking in Manaus, Brazil in December. Three-quarters of Manaus residents had already had COVID-19 by then, so the city should have been close to herd immunity from the virus. According to the CDC, the Manaus surge suggests P.1 increases the risk of reinfection in people who've already had COVID-19.
P.1 has been reported in eight countries; the US spotted its first case in Minnesota on Monday.
CAL.20C, the variant first detected in California
The US has its own homegrown variant to contend with, too.
Researchers at Cedars-Sinai Medical Center in Los Angeles first spotted a case involving a new strain, which they called CAL.20C, in July. The variant didn't appear in Southern California again until October. At the time, it didn't seem to be spreading widely in the community, but two months later the variant represented nearly one-quarter of all samples from Southern California.
The researchers think the strain may have contributed to LA's record coronavirus case surge in the late fall.
CAL.20C does have mutations in its spike protein, though it lacks the trio of mutations characterizing B.1.351 and P.1, so additional studies are needed to find out whether it spreads more easily than other existing strains, or if it can evade antibodies.
There is no sign yet that CAL.20C is deadlier than its viral counterparts, the researchers added.
Northern California, New York, Washington DC, and island countries in the Pacific Ocean have also reported cases involving CAL.20C.
Booster shots could combat variants
The spread of B.1.351, in particular, has prompted vaccine developers to start working on shots to combat virus variants. "It's really a wake-up call for us to be nimble and to be able to adjust," Fauci said.
Pfizer CEO Albert Bourla said Tuesday that his company is working on boosters to combat coronavirus variants. BioNTech, Pfizer's partner, said it could produce a new vaccine for a COVID-19 variant in about six weeks. Bourla said at Bloomberg's The Year Ahead conference on Monday that the company is working on a process to create booster shots.
Moderna, too, will soon start clinical trials to test whether giving people another booster shot of its current vaccine, or a booster shot tailor-made to neutralize B.1.351, will improve antibody responses.
"I think our technology is very well suited to actually rapidly deploy a vaccine based on the new variant," Tal Zaks, Moderna's chief medical officer, said in a recent presentation at the J.P. Morgan Healthcare Conference.
.
- There are a handful of mutated coronavirus strains worrying public health experts and vaccine developers.
- Some of these variants are more infectious, and may be deadlier or able to partially evade existing vaccines.
- Here's what to know about variants first spotted in the UK, South Africa, Brazil, and California.
While mutations are normal and most don't change a virus's behavior, sometimes these genetic errors give the virus an evolutionary leg-up against its hosts - mutations that make it more infectious, deadlier, or perhaps able to evade the protective immunity we accrue from vaccines or prior infections.
Since the fall, researchers have identified worrisome mutated strains spreading worldwide, many of which are nicknamed after where they were first detected. Many of these variants - including those from the UK, South Africa, and Brazil - share similar mutations in their spike proteins, which is what the virus uses to invade human cells. Research suggests those genetic tweaks may make it easier for the strains to infect people; some may decrease the efficacy of vaccines.
"We can see that we are going to be challenged" by the variant from South Africa, the US's leading infectious disease expert Dr. Anthony Fauci said in a press call on Friday.
Here's what to know about four coronavirus variants, where they've been spotted, and what they mean for global vaccination efforts.
B.1.1.7, the variant first spotted in the UK
Researchers spotted the first variant of concern, named B.1.1.7, in the southeastern part of the UK on September 20. By mid-December, it had overtaken all other versions of the virus in the country. B.1.1.7 is now present in 70 countries; US officials have spotted 315 cases in 28 states.
Studies have shown B.1.1.7 is between 56% and 70% more contagious than its viral predecessors. While initial evidence suggested the strain wasn't deadlier, UK officials said last week people infected with B.1.1.7 may face a higher risk of death than those who get other strains. The World Health Organization and other experts, however, cautioned more data was needed to confirm whether the variant was associated with higher mortality.
What makes B.1.1.7 so pernicious is that people infected with B.1.1.7 have higher viral loads, meaning they produce more viral particles when they're infected. Higher viral loads, multiple studies show, are associated with a higher risk of death and more severe disease.
The variant has at least 17 mutations. But two are among the most concerning because they affect its spike protein shape and may increase transmissibility: the swapping of two amino acids in the 501st position of its genome, or N501Y, and a deletion of amino acids in its 69th and 70th positions, known as the 69/70 deletion.
Virologists think vaccines will still be effective against B.1.1.7, and recent research from Pfizer-BioNTech and Moderna found that the companies' shots held up well against that variant.
Novavax, too, said Thursday its vaccine was 89% effective at preventing cases of COVID-19 based on results from a UK trial, which suggests it works against B.1.1.7.
B.1.351, the variant first found in South Africa
Experts agree the variant first detected in South Africa in October, known as B.1.351 (or 501.Y.V2), is more worrisome than the variant first found in the UK.
This variant also has the N501Y mutation, though it lacks the worrisome 69/70 deletion. But what makes this strain troublesome is two spike mutations - K417T and E484K - that are missing in B.1.1.7. E484K, in particular, has been shown to reduce how well antibodies - proteins that identify and help destroy pathogens - can recognize the coronavirus.
B.1.351 has spread to 31 countries. The US reported its first two cases of the variant, which is 50% more transmissible, Thursday.
While there's no evidence it is deadlier or causes more severe COVID-19, preliminary research published last week suggested the variant can partially evade the defenses existing vaccines build in our bodies' immune systems.
Vaccine developers Novavax and Johnson & Johnson announced Friday that their shots didn't work as well against B.1.351 than other strains. Novavax's vaccine was 89% effective at preventing COVID-19 cases in the UK, but only 49% effective in South Africa, where B.1351 is the dominant version of the virus. J&J found its shot was, on average, 66% effective; that efficacy dropped to 57% in South Africa.
Though even with the variant concerns, J&J said its vaccine was 85% effective at preventing severe COVID-19 across all geographic regions - the UK, US, Latin America, and South Africa - in which it conducted clinical trials.
Following lab research, Pfizer and Moderna, both say their vaccines will work again B.1.351. Yet recent preliminary data from Moderna showed blood samples taken from vaccinated people that were infected with B.1.351 developed six times fewer virus-neutralizing antibodies than samples exposed to other variants.
This suggests vaccines won't provide as much protection against B.1.351, and people who have already been infected with a different version of the virus could get reinfected with the new strain. (However, this lab testing doesn't take into account other elements of immunity beyond antibodies, like virus-destroying T cells.)
P.1, the variant from Brazil
A variant named P.1, with a similar genetic profile to B.1.351, is surging in Brazil. In mid-December, 42% of coronavirus cases in the Amazon region involved P.1.
Researchers first detected this strain in four travelers from Brazil who had traveled to Japan's Haneda airport outside Tokyo. Data show it's 50% more transmissible that the original version of the virus, and has the same trio of concerning spike mutations as B.1.351: N501Y, K417T, and E484K, so may also be able to evade antibodies generated from previous infections or a vaccine.
A study from earlier in January pinpointed P.1 as a variant of concerning after finding that cases had started spiking in Manaus, Brazil in December. Three-quarters of Manaus residents had already had COVID-19 by then, so the city should have been close to herd immunity from the virus. According to the CDC, the Manaus surge suggests P.1 increases the risk of reinfection in people who've already had COVID-19.
P.1 has been reported in eight countries; the US spotted its first case in Minnesota on Monday.
CAL.20C, the variant first detected in California
The US has its own homegrown variant to contend with, too.
Researchers at Cedars-Sinai Medical Center in Los Angeles first spotted a case involving a new strain, which they called CAL.20C, in July. The variant didn't appear in Southern California again until October. At the time, it didn't seem to be spreading widely in the community, but two months later the variant represented nearly one-quarter of all samples from Southern California.
The researchers think the strain may have contributed to LA's record coronavirus case surge in the late fall.
CAL.20C does have mutations in its spike protein, though it lacks the trio of mutations characterizing B.1.351 and P.1, so additional studies are needed to find out whether it spreads more easily than other existing strains, or if it can evade antibodies.
There is no sign yet that CAL.20C is deadlier than its viral counterparts, the researchers added.
Northern California, New York, Washington DC, and island countries in the Pacific Ocean have also reported cases involving CAL.20C.
Booster shots could combat variants
The spread of B.1.351, in particular, has prompted vaccine developers to start working on shots to combat virus variants. "It's really a wake-up call for us to be nimble and to be able to adjust," Fauci said.
Pfizer CEO Albert Bourla said Tuesday that his company is working on boosters to combat coronavirus variants. BioNTech, Pfizer's partner, said it could produce a new vaccine for a COVID-19 variant in about six weeks. Bourla said at Bloomberg's The Year Ahead conference on Monday that the company is working on a process to create booster shots.
Moderna, too, will soon start clinical trials to test whether giving people another booster shot of its current vaccine, or a booster shot tailor-made to neutralize B.1.351, will improve antibody responses.
"I think our technology is very well suited to actually rapidly deploy a vaccine based on the new variant," Tal Zaks, Moderna's chief medical officer, said in a recent presentation at the J.P. Morgan Healthcare Conference.
.
AD1184
Celestial
I would ask the following questions of the Stephen Lynch case: At what cycle threshold did he test positive for Covid-19? When was his last Covid-19 test, if he had had one before? Did he develop symptomatic disease, or did he only test positive? Is he, or was he ever, infectious to other people? (The last question may not be answerable.)These vaccination efforts may be futile, this infection reported below could be one of the new variants that are more resistant to our vaccines and could be only the beginning of more similar cases arising...
Stephen Lynch is 65 years old, it is likely that this age group does not have the same 92-95% effectiveness averaged across all age groups. Between 1 in 20, and 1 in 12 people will not be covered by the vaccine after two doses. They, along with those who can't or won't be vaccinated, will need to rely upon a herd immunity effect from the rest of the population being vaccinated. Nevertheless, Stephen Lynch may in fact be getting protection from the vaccine, which may have prevented him from having a more severe illness that could have put him in the hospital, or worse, cost him his life.
For example, it is thought that at three weeks after a single does of the Oxford-AstraZeneca vaccine, there is 100% protection--or very nearly--against hospitalization due to Covid.
Last edited:
nivek
As Above So Below
I plan to get the Johnson & Johnson vaccine when available for me...They have stated something similar that although it's still possible to get sick with covid even after being vaccinated with their product, there's a good chance the vaccine will keep people from going into the hospital...
...
...
AD1184
Celestial
The UK epidemic now seems to be coming down from a peak in infections at the start of the year. Deaths peaked at 1,324 occurring on the 18th of January (by date of death, not date of report; the per capita equivalent of around 6,460 deaths occurring in one day in the US). We remain in a rather severe lockdown, which does at least seem to be having an effect in reducing the rate of transmission of the mutant strain of the virus. We are down to fewer than 30,000 new cases a day on average, from a peak of more than 60,000 in early January. The rate of new deaths is still likely around 1,000 per day.
More than 600,000 vaccine doses were given yesterday. Nearly 9,000,000 people in total have had at least the first dose, as of yesterday, which is more than 13% of the population. Some of my older relatives have already been vaccinated. An elderly couple, who are family friends, are both in hospital with the disease. They had been isolating at home, but also had a carer coming around regularly, which is an obvious transmission route.
More than 600,000 vaccine doses were given yesterday. Nearly 9,000,000 people in total have had at least the first dose, as of yesterday, which is more than 13% of the population. Some of my older relatives have already been vaccinated. An elderly couple, who are family friends, are both in hospital with the disease. They had been isolating at home, but also had a carer coming around regularly, which is an obvious transmission route.
Last edited:
coubob
Celestial
Here in Oklahoma, our pastor has spoke at 11 funerals this month. including his own mothers. I sure our numbers here get better here, and all over for that matter. I am kinda shocked how high Oklahoma is on the list. My wife was called to get the shot than they called back saying only 65+, the doc had tried to get her through with all her things wrong with her, personly i`m leary of getting the shot .
AD1184
Celestial
Portugal is currently the nation hardest-hit by Covid, in terms of the number of new Covid cases per day per capita.
Coronavirus Pandemic Data Explorer
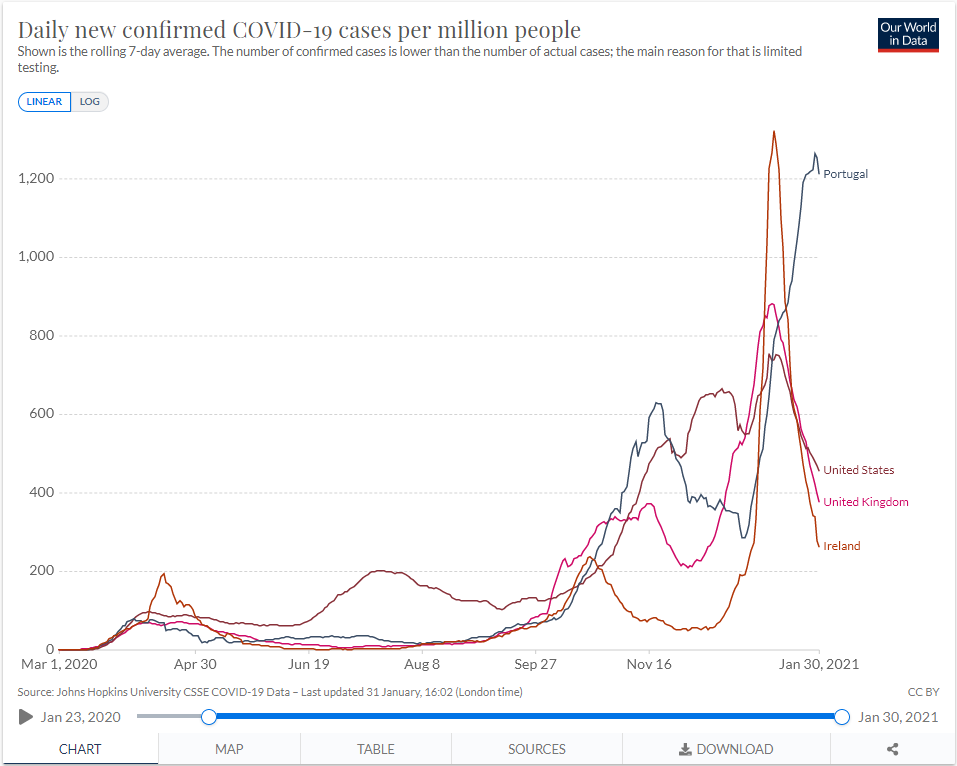
Ireland had a huge peak in Covid cases beginning in early January, due to the arrival of the British variant, but they have suppressed this outbreak with a strict lockdown. Now Portugal is seeing a surge in cases driven by the arrival of the British variant. Apparently a large number of both Britons and Portuguese travelled from Britain to Portugal for Christmas, and Portugal took action far too late to do anything about it. Portugal also has close links with Brazil and South Africa, where other mutant strains have originated, and a significant traffic in people between those nations.
Coronavirus Pandemic Data Explorer
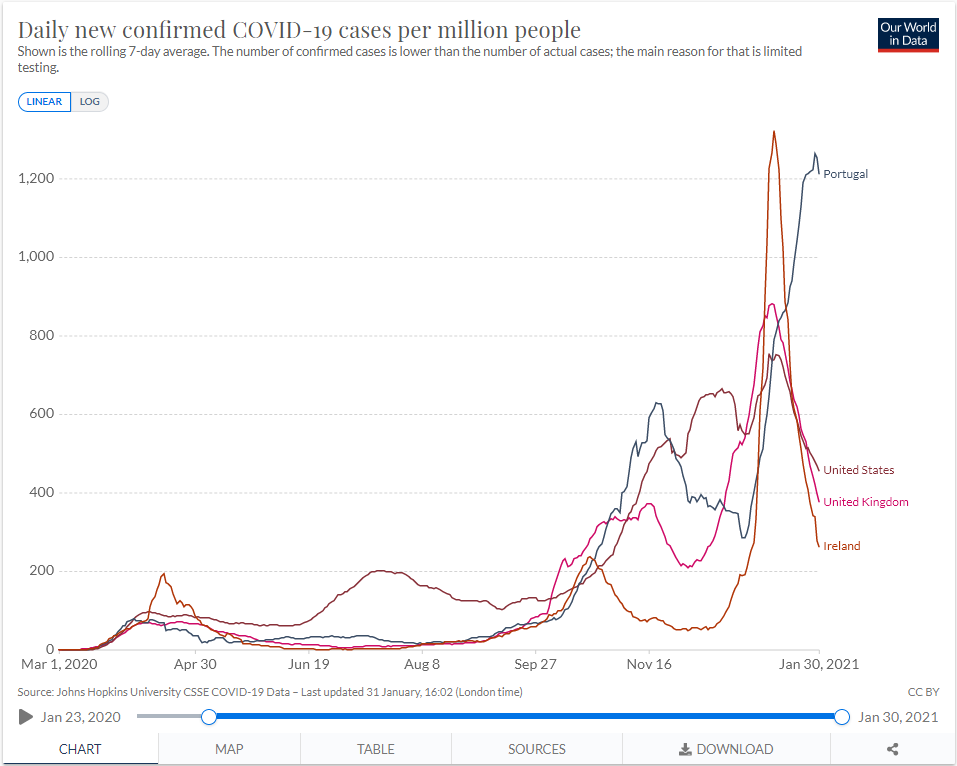
Ireland had a huge peak in Covid cases beginning in early January, due to the arrival of the British variant, but they have suppressed this outbreak with a strict lockdown. Now Portugal is seeing a surge in cases driven by the arrival of the British variant. Apparently a large number of both Britons and Portuguese travelled from Britain to Portugal for Christmas, and Portugal took action far too late to do anything about it. Portugal also has close links with Brazil and South Africa, where other mutant strains have originated, and a significant traffic in people between those nations.
nivek
As Above So Below
'That hurricane is coming’: expert warns US to brace for virulent Covid strain
A leading infectious disease expert predicted on Sunday that the deadlier British variant of Covid-19 will become the dominant strain of the virus in the US and could hit the country like a hurricane.
The worrying forecast came as the total of confirmed infections in the US passed the 26m mark, with the death toll advancing steadily towards the grim milestone of half a million after on Sunday surpassing the total of 440,000, by far the highest in the world according to data gathered by the Johns Hopkins University coronavirus research center.
Epidemiologist Michael Osterholm, who served on Joe Biden’s transition coronavirus advisory board after the Democratic victory in the 2020 election, and is director of the center for infectious disease research and policy at the University of Minnesota, warned America to brace for the spread of the virulent strain this spring.
“The surge that is likely to occur with this new variant from England is going to happen in the next six to 14 weeks, Osterholm told NBC’s Meet the Press show on Sunday morning.
He urged the new administration to move faster with plans to get as many people as possible in the US vaccinated, at least with their first dose, especially those aged over 65, in order to try and stave off the worst exacerbation by variants of the ongoing crisis.
“That hurricane is coming,” Osterholm told NBC.
British prime minster Boris Johnson has warned that the new UK variant may be 30% more deadly than the original virus. The strain was first identified in the US in late December but is thought to have been present there as early as October.
Osterholm indicated that if leaders across the US cannot stay ahead of the more contagious and more virulent UK strain a disaster is bearing down in the form of a new and rapid surge of infections, in a pandemic that has been out of control since it hit the US more than a year ago.
“If we see that happen…we’re going to see something like we have not yet seen in this country…I see that hurricane Category 5, 450 miles offshore,” Osterholm told NBC.
The US Centers for Disease Control and Prevention (CDC) has reported that, so far, almost 50 million vaccine doses have been distributed and about 30m of those administered to patients, out of a US population in excess of 320m.
.
A leading infectious disease expert predicted on Sunday that the deadlier British variant of Covid-19 will become the dominant strain of the virus in the US and could hit the country like a hurricane.
The worrying forecast came as the total of confirmed infections in the US passed the 26m mark, with the death toll advancing steadily towards the grim milestone of half a million after on Sunday surpassing the total of 440,000, by far the highest in the world according to data gathered by the Johns Hopkins University coronavirus research center.
Epidemiologist Michael Osterholm, who served on Joe Biden’s transition coronavirus advisory board after the Democratic victory in the 2020 election, and is director of the center for infectious disease research and policy at the University of Minnesota, warned America to brace for the spread of the virulent strain this spring.
“The surge that is likely to occur with this new variant from England is going to happen in the next six to 14 weeks, Osterholm told NBC’s Meet the Press show on Sunday morning.
He urged the new administration to move faster with plans to get as many people as possible in the US vaccinated, at least with their first dose, especially those aged over 65, in order to try and stave off the worst exacerbation by variants of the ongoing crisis.
“That hurricane is coming,” Osterholm told NBC.
British prime minster Boris Johnson has warned that the new UK variant may be 30% more deadly than the original virus. The strain was first identified in the US in late December but is thought to have been present there as early as October.
Osterholm indicated that if leaders across the US cannot stay ahead of the more contagious and more virulent UK strain a disaster is bearing down in the form of a new and rapid surge of infections, in a pandemic that has been out of control since it hit the US more than a year ago.
“If we see that happen…we’re going to see something like we have not yet seen in this country…I see that hurricane Category 5, 450 miles offshore,” Osterholm told NBC.
The US Centers for Disease Control and Prevention (CDC) has reported that, so far, almost 50 million vaccine doses have been distributed and about 30m of those administered to patients, out of a US population in excess of 320m.
.
Dr_Doom
Honorable
These vaccination efforts may be futile, this infection reported below could be one of the new variants that are more resistant to our vaccines and could be only the beginning of more similar cases arising...
...
Congressman who had second COVID-19 vaccine dose tests positive for virus
A Massachusetts congressman tested positive coronavirus just a few weeks after receiving the second of two doses of the Pfizer vaccine.
Molly Rose Tarpey, the communications director for Rep. Stephen Lynch, told Fox News on Saturday that the lawmaker received the second jab and tested negative for COVID-19 before attending President Biden's inauguration in Washington, D.C., on Jan. 20.
On Friday, Lynch, D-Mass., received a positive test result for coronavirus after a staff member in his Boston office also contracted the virus.
(More on the link)
.
Doh... why do people think the vaccine is going to stop them getting the virus. That’s not how it works lol.

